
Dr Penny Burns
April 9, 2020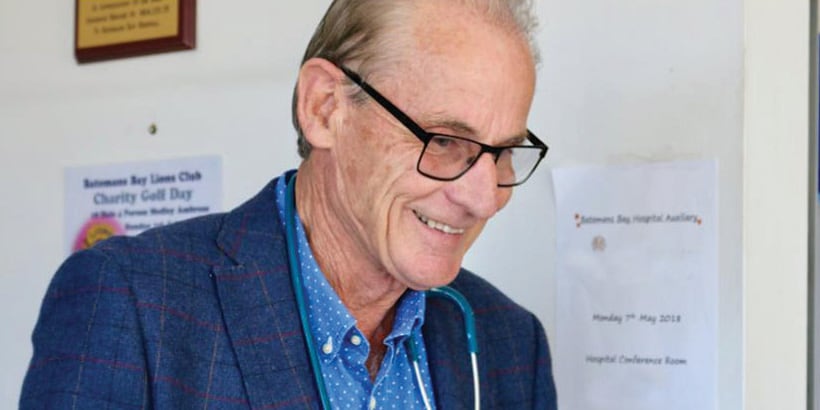
Fences to Build
April 9, 2020FEATURE
Surf Beach Surgery general practitioner, Dr James Langley, recounts his experience over New Year’s Eve and the subsequent impact of the bushfires on healthcare delivery in the area.
Late last year, Dr James Langley recalls walking around his rural property on the South Coast and remarking to his son that he had never seen the bush so dry.
“It was really weird – it was like walking on yellow cellophane.”
Having experienced the 1969 Lara bushfires as a kid, the threat of bushfires has always been at the back of his mind. So when he purchased a rural property near Batemans Bay, he did as much hazard reduction around his property as possible. Despite these preparations, when the bushfires threatened the South Coast just after Christmas, his plan was to get out early.
On 31 December, Dr Langley woke at 4am.
“I woke up early and someone had sent me a link to a satellite map, which wasn’t working most of the time, but it just happened to be working and I could see there were already hot spots in Batemans Bay.”
By 4.45am Dr Langley and his family, along with his brother and his kids, were on the Princes Highway. About 6am they were travelling through burnt areas when they received warning that Mogo was on fire. At that point they cut across Kangaroo Valley and hit the Hume Highway. They stopped for breakfast near Marulan. When Dr Langley checked the bushfire map again it showed the area they were in was under threat and so they kept going until they reached Canberra.
After taking his son, who was unwell at the time, to Canberra Hospital and ensuring his family was safe, the Surf Beach general practitioner got in contact with Batemans Bay Hospital where, until recently, he had served as a VMO for 16 years.
“I wanted to see if I could come back and the doctor in charge of the emergency response said ‘yes, you can and I can appoint you, but I want you in Moruya, not Batemans Bay, because we’re expecting major casualties tomorrow’.”
This was Friday 3 January. Dr Langley consulted the RFS fire maps again which revealed large fires to the North and South of Moruya, which were expected to merge on Saturday.
“It was completely unpredictable at that point what would happen to Moruya, because Moruya has farm land but it also has bush adjoining properties and the hospital is not particularly well defended,” Dr Langley recalls.
He was assured Moruya Hospital had a bunker, so he left Canberra to join medical professionals there.
“I was a bit shocked at how unprepared the hospital was in that there was only two externally fixed fire hoses at Moruya Hospital. I thought there’d be a fire truck at the hospital, but they couldn’t release one to just sit there, and the RFS was busy.”
Expecting mass casualties, the team at Moruya Hospital set up triage areas of the hospital based on traditional triage categories.
Fortunately, there was Southerly wind change, and the area was spared further destruction.
On Sunday 5 January, in an effort to stem the flow of patients going into the emergency department, Dr Langley ran an outreach clinic at the Moruya evacuation centre, on the basketball court. He followed that by running a similar clinic at Batemans Bay, where he was accompanied by community health nurses from NSW Health, and liaised with St John’s Ambulance personnel who were providing first aid at the evacuation centres.
Dr Langley then visited aged care facilities in Batemans Bay.
“It was pretty harrowing seeing frail, elderly people who had spent time on the beach, elderly people who had slept on the beach, elderly people who had slept on the concrete floor of surf clubs, people who had slept in their cars…”
Some of the aged care facilities in the area had been were evacuated, while newer facilities that had fire-resistant areas of the building, with concrete walls and concrete ceilings, were able to safely house their residents in one area.
“But they didn’t have power, they didn’t have telephones, they didn’t have mobile phones, so it was a real problem trying to get messages out,” Dr Langley says.
“One of the aged care nurses had actually told me they had fire on three sides – and at one point she was out the back with the garden hose trying to wet down the scrub until the RFS arrived and the helicopters started water bombing. So, it was a very near thing.”
By Monday 6 January, Dr Langley decided to try and open general practices and pharmacies in Batemans Bay. While he was able to contact doctors, he couldn’t reach pharmacists to see who would be able to open – given that there was no power.
Fortunately, he had the telephone number for a pharmacist who had relocated to Canberra and after making contact, he was able to get phone numbers for other pharmacists in the Batemans Bay area.
Soon after, they were able to broadcast on ABC Radio which surgeries and pharmacies were open, as well as alerting the community through Facebook.
Dr Langley says there was no power at Surf Beach Surgery, “but we were just able to use the window light and hand write scripts.” Likewise, the pharmacy adjacent to the surgery was able to dispense medication without power, which was restored to the area on 7 January.
At the time The NSW Doctor spoke with Dr Langley, he was aware of 17 families who attended his surgery who had lost their homes, in addition to a colleague at the surgery, as well as three other doctors in the Batemans Bay area who had their homes severely damaged by fires.
“It’s really hit the community. Everybody knows somebody who’s lost their home and everybody is really quite traumatised. I just saw an elderly couple and she still goes into a panic whenever a helicopter goes overhead.”
He adds, “the people who have been particularly hard hit are the elderly, people who have lost their homes, people who have already had mental health problems, war veterans, people with early dementia.”
Dr Langley says almost every consultation turns into a counselling session with patients.
“We were already in an area that has a shortage of doctors, so it’s a long wait for appointments and now we’re just having to work that bit harder.”
In relaying his experiences, Dr Langley admitted the initial adrenaline was turning into exhaustion.
“It was full on. I found 99% of the time I was alright, but 1% of the time I just felt like crying actually.”
Looking to the future, he says: “I think it’s going to take months for people to feel normal and it’s going to take years for the area to actually be normal.”
Editor’s note: Since the initial bushfire threat to South Coast areas surrounding Moruya Hospital, the area faced two more battles. The Clyde Mountain fire came within 150m of the hospital.

